Yep, it is very well known that the sugar coating (aka glycosylation) of viruses makes them invisible to the immune system, a strategy so effective that like in the case of HIV, whose spike is almost entirely covered by glycans, makes it so difficult to target by the human immune system.
Unsurprisingly, coronaviruses such as SARS, MERS, and SARS-CoV-1(2) not only benefit from this evolutionary strategy but there is evidence now that sugars provide stability to their spikes to be effective binders by glueing the spike chains, hence making them infectious.
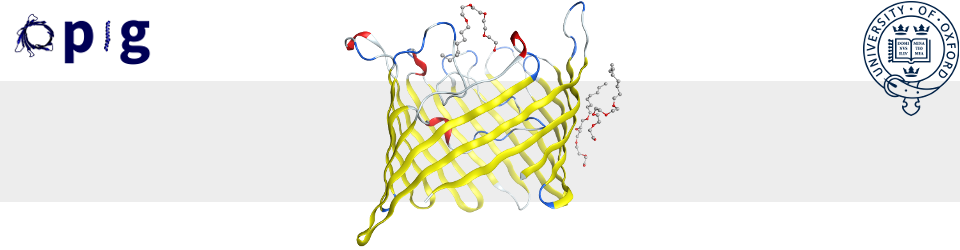
This is the major finding of this paper that introduces very interesting results from all-atom MD simulations of a fully glycosylated model of the SARS-CoV-2 spike protein embedded in a realistic viral membrane. Researchers aimed to look into the stability of the protein spike (A, B, and C) chains in the “open” and “closed” conformation and how these changed upon key residue mutations to test how glycans sitting in the inter-chain space affect stability. It also aimed at quantifying glycans’ shielding effect from molecules ranging from 2 to 15 Angstroms, i.e., from small-sized to peptide- and antibody-sized molecules.
Analysis showed that glycans provide a protective layer in the “down” conformation of the Receptor Binding Domain (RBD) and in particular N165 and N234 chain-A residues and their glycans provide structural stability to the RBD in the “up” conformation, which mediates binding to the Angiotensin-Converting Enzyme 2 (ACE2) receptor – the first entry point in humans. Upon mutation of N165 and N234 and removal of their glycans, the stability of the spike in its open conformation decreases, making chains more loosely bound.
Glycans attached to these key residues provide inter-chain stability for the spike by forming extended hydrogen bond networks that link to residues from other chains, explaining the increased flexibility of the spike chains in their absence. Moreover, thin-layer Interferometry experiments measuring binding to the ACE2 receptor of mutant variants of the spike protein show that mutant variants lead to lower binding affinity than the original spike and a control. Hence, confirming the stabilising role of the mutated residues and their glycans.
Accessible Surface Area (ASA) measurements for various probe radii were a key methodology in the study to quantify the shielding coverage that glycans have on the spike. ASA figures showed that the head of the spike is more exposed to large molecules, such as neutralising antibodies, in contrast to the stalk, which seems more accessible to smaller molecules. Reported epitopes in the literature (Table S2 in the Supplement) are consistent with these findings, hence this is why most antibody therapies target the spike’s head.
In particular, the RBD in its “up” conformation is more exposed than in the “down” conformation, which is when glycans bury the Receptor Binding Motif (RBM) – the part of the RBD that sticks to ACE2, hence making it less exposed to biding molecules.
The paper argues in general terms that their findings can be exploited in vaccine and therapy development, however, it is rather unclear how in practice to do so, and not even a slight hint is provided. Despite this, the paper makes an interesting read.